Parasites in Humans: Types, Symptoms, and Best Treatments

Parasites in humans are living organisms that survive by feeding on a host, often causing illness in the process. Unlike bacteria or viruses, which multiply inside the body, human parasites such as intestinal worms, protozoan parasites, and ectoparasites live off the nutrients and blood of their host, sometimes for years if left untreated. These infections, known as parasitic diseases can affect nearly every system in the body, from the digestive tract and bloodstream to the skin, liver, lungs, and even the brain.
Globally, parasitic infections are a serious health concern. The World Health Organization estimates that billions of people suffer from helminth infections, malaria (Plasmodium), or protozoa like Giardia lamblia and Entamoeba histolytica. Even in the United States, where sanitation is generally high, cases of pinworms, tapeworms (Taenia), scabies mites, and head lice remain common, especially among children. Tropical parasites in travelers are also increasingly diagnosed in those returning from endemic regions. These diseases can cause fatigue, abdominal pain, diarrhea, anemia, skin rash, weight loss, and nutritional deficiencies, making them a major issue for both public health and clinical parasitology.
Parasites spread through many routes, including fecal-oral transmission from contaminated food and water, vector-borne diseases such as malaria from mosquito bites, direct contact with infected individuals, or exposure to contaminated soil and undercooked meat. Poor sanitation, unsafe water, close person-to-person spread, and pet ownership also increase risk. For travelers, tropical medicine specialists often stress travel precautions and prophylactic treatment to avoid infection abroad.
Understanding the types of parasites, their symptoms, and the best treatments is essential for protecting your health and preventing long-term complications.
What Are Human Parasites?
In simple terms, human parasites are organisms that live in or on the body and depend on it for survival, often causing harm in the process. Unlike bacteria, which can sometimes be beneficial (like gut flora), or viruses, which replicate inside host cells, parasites usually feed on nutrients, blood, or tissues, leading to parasitic infections that range from mild discomfort to life-threatening disease.
Types of Parasites in Humans
- Protozoa (Single-Celled Parasites)
These protozoan parasites are microscopic but capable of serious illness.
Examples include:
- Giardia lamblia → causes giardiasis, a common waterborne parasite leading to prolonged diarrhea.
- Entamoeba histolytica → responsible for amebiasis, often linked to poor sanitation.
- Toxoplasma gondii → linked to toxoplasmosis, which can affect the brain and eyes, and is especially dangerous during pregnancy.
These typically spread through contaminated water, undercooked meat, or fecal-oral transmission.
2. Helminths (Parasitic Worms)
Larger, multicellular organisms are often called intestinal parasites or tissue parasites, depending on where they live in the body.
Examples include:
- Roundworms (Ascaris) → cause digestive issues, bloating, and malnutrition.
- Pinworms (Enterobius vermicularis) → a common childhood infection leading to anal itching and sleep disturbances.
- Tapeworms (Taenia) → can grow several feet inside the intestines and cause nutritional deficiencies.
- Flukes (Trematodes) → less common in the U.S. but widespread in Asia and Africa, affecting the liver and lungs.
- Roundworms (Ascaris) → cause digestive issues, bloating, and malnutrition.
- Helminth infections are a leading cause of anemia, abdominal pain, and chronic digestive problems.
3. Ectoparasites (External Parasites)
These arthropod parasites live on the skin or hair and cause itching, rashes, and discomfort.
Examples include:
- Scabies mites → burrow into skin, causing intense itching and rashes.
- Head lice → infest the scalp, spreading easily in schools and crowded areas.
- Bed bugs, fleas, and ticks → can cause skin irritation and, in some cases, transmit other vector-borne diseases.
- Scabies mites → burrow into skin, causing intense itching and rashes.
Parasites vs. Bacteria and Viruses: Key Differences
- Parasites are organisms that live at the expense of a host and can be either microscopic (protozoa) or visible to the naked eye (worms, lice).
- Bacteria are single-celled microbes; some are harmful (like Salmonella), but many are harmless or beneficial.
- Viruses are non-living particles that invade cells to reproduce and rely entirely on the host’s cellular machinery.
- Unlike bacteria and viruses, parasites often have complex life cycles, sometimes involving multiple hosts, which makes parasite treatment more challenging.
Common Parasitic Infections in Humans
Parasitic infections can affect different parts of the body, from the digestive system to the skin, blood, and even the brain. Some are more common in tropical regions with poor sanitation, while others like pinworms and head lice are still widespread in developed countries, including the U.S.
1. Intestinal Worms (Helminth Infections)
- Roundworms (Ascaris lumbricoides): Often found in areas with poor sanitation. They cause abdominal pain, bloating, constipation, and nutritional deficiencies.
- Pinworms (Enterobius vermicularis): The most common intestinal parasite in children in the U.S. They lead to intense anal itching, especially at night, and sleep disturbances.
- Hookworms: These worms attach to the intestinal lining, causing anemia, fatigue, and digestive problems. Infection usually happens when walking barefoot on contaminated soil.
2. Malaria (Plasmodium Species)
- Caused by blood parasites of the genus Plasmodium, spread by mosquito bites.
- Symptoms include fever, chills, sweating, anemia, and fatigue.
- While malaria is rare in the U.S., it is still one of the deadliest tropical parasites in travelers and endemic populations in Africa, Asia, and South America.
3. Giardiasis and Amebiasis (Protozoan Infections)
- Giardia lamblia → causes giardiasis, a common waterborne parasite infection. It leads to prolonged diarrhea, bloating, nausea, and fatigue.
- Entamoeba histolytica → responsible for amebiasis, which may cause severe dysentery, abdominal pain, and liver abscesses.
- These infections are linked to contaminated water and poor hygiene practices.
4. Toxoplasmosis (Toxoplasma gondii)
- Spread through undercooked meat, contaminated water, or infected cats.
- Often asymptomatic, but in high-risk groups (pregnant women, immunocompromised patients) it can cause serious brain, eye, or congenital infections.
5. Tapeworm Infections (Taenia Species)
- Tapeworms are intestinal parasites that can grow several feet long inside the body.
- Infection occurs by eating undercooked or contaminated meat.
- Symptoms may include weight loss, nutritional deficiencies, abdominal pain, and segments of the worm visible in stool.
6. Scabies and Lice Infestations (Ectoparasites)
- Scabies mites burrow under the skin, leading to intense itching, rashes, and secondary infections from scratching.
- Head lice are common in school-aged children, spreading easily through close contact.
- While not life-threatening, these skin parasites cause significant discomfort and social stigma.
Regional vs. Global Burden
- Worldwide: Billions suffer from intestinal worms, malaria, giardiasis, and ectoparasitic infestations, especially in areas with poor sanitation and contaminated water.
- United States: While tropical diseases are less common, pinworms, Giardia, scabies, head lice, and tapeworms are still frequently diagnosed. Increasing international travel and migration also raise the risk of exposure to tropical parasitic diseases.
How Do People Get Parasites?
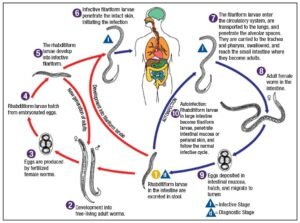
Parasites don’t just appear out of nowhere, there are specific ways they enter the human body. Understanding these transmission routes is key to both prevention and treatment.
1. Contaminated Food and Water
One of the most common ways parasites spread is through eating undercooked meat (such as pork, beef, or fish) or drinking unclean water. For example:
- Tapeworms often come from raw or undercooked beef or pork.
- Giardia and Entamoeba histolytica thrive in untreated drinking water.
This is why safe food preparation and clean drinking water are essential to avoiding infection.
2. Poor Hygiene and Sanitation
Parasites flourish in areas with inadequate sanitation. When people don’t wash hands after using the toilet or before meals, eggs and cysts can easily spread.
- Pinworms, for instance, spread quickly among children in households and schools.
- Soil contaminated with human or animal feces may harbor roundworms and hookworms, which can enter the body through ingestion or skin contact.
3. Close Contact and Person-to-Person Transmission
Some parasites can spread directly from one person to another:
- Scabies mites pass through skin-to-skin contact.
- Head lice spread via shared items like hats, combs, or bedding.
- Certain protozoa, such as Trichomonas vaginalis, can be sexually transmitted.
This makes personal hygiene and avoiding the sharing of personal items very important.
4. Travel to Endemic Areas
International travelers visiting tropical or subtropical regions may be exposed to parasites uncommon in the U.S. or Europe.
- Malaria (Plasmodium species) is a major concern in Africa, South Asia, and parts of South America.
- Visitors may also encounter schistosomiasis and leishmaniasis in regions with poor water management or high insect vector populations.
Travelers should always research health risks and consider prophylactic medications before visiting endemic regions.
5. Zoonotic Infections (From Pets and Animals)
Parasites don’t just come from people, animals can carry them too.
- Cats can transmit Toxoplasma gondii through contaminated litter.
- Dogs may carry tapeworms or roundworms that can infect humans.
- Farm animals, fish, and even wild game may harbor parasites transmissible to humans.
Regular veterinary care for pets and good hygiene after handling animals can reduce these risks.
Symptoms of Parasitic Infections
Parasites affect people in different ways depending on the type of organism and the part of the body they invade. Some infections are mild and go unnoticed, while others cause severe and even life-threatening complications. Recognizing the symptoms early is critical for timely treatment.
General Symptoms of Parasitic Infections
Many parasitic diseases share overlapping symptoms that can easily be mistaken for other conditions:

- Persistent fatigue and weakness
- Abdominal pain, cramping, or bloating
- Diarrhea or nausea that lingers for days to weeks
- Unexplained weight loss despite normal eating habits
- Itching or skin irritation (especially around the anus or scalp)
These general signs should not be ignored, especially if they persist after travel or exposure to risk factors.
Specific Symptoms by Parasite Type
Worm Infections (Helminths)
- Pinworms → intense anal itching, especially at night
- Roundworms or hookworms → bloating, abdominal discomfort, visible worms in stool
- Tapeworms → weight loss, abdominal pain, sometimes segments of the worm in stool
Protozoan Infections
- Giardia or Entamoeba → prolonged diarrhea, dehydration, greasy or foul-smelling stools
- Toxoplasmosis → flu-like symptoms, swollen lymph nodes, muscle aches (dangerous in pregnancy and immunocompromised patients)
Malaria (Plasmodium species)
- Recurring fever cycles with chills and sweating
- Severe headache, night sweats, and body aches
- If untreated, complications may include anemia, seizures, or organ damage
Ectoparasites (Scabies & Lice)
- Scabies → intense itching, especially at night, small red bumps, burrow-like skin rashes
- Head lice → crawling sensation on the scalp, visible nits (eggs) attached to hair strands
- Body lice → red bite marks, itching, and secondary bacterial skin infections
When to See a Doctor Immediately
Seek urgent medical care if you notice:
- High fever with chills after recent travel
- Severe or bloody diarrhea lasting more than a few days
- Rapid weight loss or extreme fatigue
- Intense skin rashes with signs of infection (pus, spreading redness)
- Neurological symptoms such as seizures, confusion, or vision problems (possible in toxoplasmosis or cysticercosis)
Diagnosis of Human Parasites
Accurate diagnosis is the cornerstone of effective parasite treatment. Since many parasitic infections mimic bacterial or viral illnesses, proper testing is essential to avoid misdiagnosis and unnecessary medication.
Common Diagnostic Tests for Parasitic Infections
1. Stool Examination (Ova and Parasite Test)
The most widely used test for intestinal parasites such as Giardia, Ascaris, Hookworm, and Tapeworms. Lab specialists look for eggs, larvae, or cysts under a microscope.
2.Blood Tests
Useful for detecting blood-borne parasites like Plasmodium (malaria), Toxoplasma gondii, or Trypanosoma. These may include:
- Microscopic blood smears for malaria diagnosis
- Serology tests that detect antibodies or antigens
- PCR (Polymerase Chain Reaction) for advanced parasite DNA detection
- Microscopic blood smears for malaria diagnosis
3. Skin Scrapings and Biopsy
Performed when ectoparasites like scabies mites, lice, or fleas are suspected. In some cases, a small skin biopsy helps identify tissue-dwelling parasites.
4. Imaging Studies
- Ultrasound, CT scan, or MRI can reveal cysts or lesions caused by parasites such as Echinococcus (hydatid cysts) or Taenia solium (neurocysticercosis).
- Imaging is especially important when parasites affect organs like the brain, liver, or lungs.
- Ultrasound, CT scan, or MRI can reveal cysts or lesions caused by parasites such as Echinococcus (hydatid cysts) or Taenia solium (neurocysticercosis).
Why Accurate Diagnosis Matters
- Guides proper treatment → Different parasites require specific antiparasitic drugs (e.g., albendazole for worms, antimalarials for malaria).
- Prevents complications → Misdiagnosis can delay therapy and worsen the infection.
- Avoids drug resistance → Overuse of antiparasitic drugs without lab confirmation may contribute to resistance.
Key takeaway: If you suspect a parasitic infection, don’t rely on guesswork or home remedies. Consult a healthcare provider for the right diagnostic tests before starting treatment.
Best Treatments for Human Parasites
Treating parasitic infections requires targeted antiparasitic drugs, since each parasite type responds to specific medications. Self-medicating is risky because the wrong drug or the wrong dosage may not only fail but also lead to drug resistance or side effects.
1. Antihelminthics (Worm Infections)
Used for intestinal worms such as roundworms, pinworms, hookworms, and tapeworms.
- Albendazole & Mebendazole → kill or immobilize worms by starving them of nutrients.
- Ivermectin → effective for strongyloidiasis, river blindness (Onchocerca), and scabies in some cases.
2. Antiprotozoals (Protozoan Parasites)
Work against microscopic parasites that invade the intestines, blood, or tissues.
- Metronidazole & Tinidazole → treat Giardia lamblia, Trichomonas vaginalis, and Entamoeba histolytica.
- Nitazoxanide → often prescribed for Cryptosporidium infections and giardiasis.
3. Antimalarials (Malaria Treatment)
Target parasites of the Plasmodium species.
- Chloroquine → effective where resistance is low.
- Artemisinin-based combination therapies (ACTs) → gold standard in regions with chloroquine-resistant malaria.
4. Ectoparasiticides (Skin Parasites)
Used for lice, scabies, fleas, and mites.
- Permethrin cream/shampoo → first-line treatment for scabies and head lice.
- Topical or oral ivermectin → alternative for resistant scabies and severe infestations.
Prescription vs. Over-the-Counter Options
- Prescription-only: most antiparasitic drugs (albendazole, ivermectin, metronidazole, ACTs).
- OTC options: some lice shampoos (permethrin-based), but effectiveness varies.
Always confirm diagnosis before choosing treatment, many OTC “parasite cleanses” are ineffective or unsafe.
Quick-Reference Parasite Treatment Table
Parasite/Disease | Drug of Choice | Alternative(s) |
Roundworms, Hookworms, Pinworms | Albendazole, Mebendazole | Pyrantel pamoate (OTC for pinworms) |
Tapeworms (Taenia) | Albendazole, Praziquantel | Niclosamide (in some regions) |
Giardiasis | Metronidazole, Tinidazole | Nitazoxanide |
Amebiasis (Entamoeba) | Metronidazole | Tinidazole |
Malaria (Plasmodium) | Chloroquine, ACTs | Atovaquone-proguanil |
Cryptosporidiosis | Nitazoxanide | Supportive hydration |
Scabies | Permethrin cream | Oral Ivermectin |
Head lice | Permethrin shampoo | Malathion lotion |
Safety & Side Effects of Antiparasitic Treatments
While antiparasitic drugs are generally effective, they can cause side effects that vary depending on the medication, the parasite being treated, and the patient’s health condition. Understanding potential risks helps ensure safe and effective parasite treatment.
Common Mild Side Effects
These are usually temporary and improve as treatment continues:
- Digestive issues → nausea, vomiting, diarrhea, bloating, abdominal pain.
- Neurological effects → mild headache, dizziness, fatigue.
- Skin reactions → itching, rash, mild irritation (more common with topical treatments like permethrin).
Serious Risks (Less Common but Important)
Some patients may experience more severe reactions:
- Allergic reactions → swelling, difficulty breathing, hives (requires urgent medical care).
- Liver toxicity → elevated liver enzymes, jaundice (linked to albendazole, mebendazole, and metronidazole).
- Kidney effects → rare but possible with certain drugs.
- Neurological issues → seizures, confusion, or numbness (seen with prolonged or high-dose therapy).
- Drug resistance → improper use or incomplete treatment can make parasites harder to eliminate in the future.
Special Considerations
Certain groups need extra caution when taking parasitic disease medications:
- Children → dosing depends on age and weight; some drugs are not approved for very young kids.
- Elderly → more sensitive to side effects due to reduced liver/kidney function.
- Pregnant women → some antiparasitics (e.g., albendazole, ivermectin) are not considered safe in pregnancy; medical supervision is essential.
- Immunocompromised patients → those with HIV, cancer, or post-transplant may require longer or combination therapy.
Natural & Supportive Remedies
While prescription antiparasitic drugs are the mainstay of treatment, supportive remedies and lifestyle measures can help recovery and reduce the risk of reinfection. Some natural approaches are backed by evidence, while others remain myths.
Probiotics and Gut Health
- Why they matter: After intestinal parasitic infections (like giardiasis or amebiasis), the gut microbiome often becomes unbalanced.
- Probiotics (e.g., Lactobacillus, Bifidobacterium) may help restore healthy gut flora, improve digestion, and strengthen natural defenses.
- Foods like yogurt, kefir, kimchi, and other fermented foods can support gut recovery.
Hygiene and Dietary Habits
Good habits can reduce recurrence of parasitic infections:
- Wash fruits and vegetables thoroughly.
- Avoid undercooked or raw meat and fish (to prevent tapeworms and toxoplasmosis).
- Drink safe, purified water—especially when traveling.
- Practice regular handwashing, especially after handling pets or soil.
Myths vs. Evidence-Based Natural Remedies
- Garlic, pumpkin seeds, papaya seeds → Some lab studies show mild antiparasitic effects, but these are not strong enough to replace medications. They may serve as supportive measures alongside medical therapy.
- “Parasite cleanses” or herbal detox kits → Marketed heavily online, but most lack scientific evidence and may even be harmful.
- Evidence-based measures → A nutrient-rich diet, proper hydration, and maintaining good hygiene are proven to help the body recover and prevent reinfection.
Preventing Parasitic Infections
The best way to avoid parasitic diseases is through prevention, since many infections are easier to stop than to treat. Preventive strategies apply at the individual, household, and community level.
Food Safety and Proper Cooking
- Wash raw fruits and vegetables thoroughly before eating.
- Cook meat, poultry, and seafood to safe internal temperatures to kill parasites like tapeworms and Toxoplasma gondii.
- Avoid raw or undercooked fish, especially in areas where parasites are common.
Clean Water Practices
- Drink only purified, boiled, or bottled water in areas where water contamination is a risk.
- Avoid ice cubes made from unclean water.
- Use safe water for brushing teeth and preparing food while traveling.
Personal Hygiene
- Wash hands with soap and water before eating, after using the bathroom, and after contact with pets or soil.
- Keep fingernails short and clean to reduce the spread of pinworms and intestinal parasites.
- Teach children proper hygiene habits, since schools and daycares are hotspots for parasite transmission.
Travel Safety Precautions
- Take prophylactic medications if traveling to malaria-endemic regions (consult a travel medicine specialist).
- Sleep under insecticide-treated mosquito nets.
- Stick to bottled or boiled water, and avoid raw street food.
- Wear protective clothing and use insect repellent to reduce vector-borne parasite risks like malaria and leishmaniasis.
Community-Level Strategies
- Improve sanitation infrastructure to limit fecal-oral transmission of intestinal parasites.
- Control insect vectors (mosquitoes, ticks, flies) through spraying, bed nets, and environmental management.
- Promote public health education on parasite prevention, safe food handling, and water hygiene.
Special Populations
Some groups are at higher risk of complications from parasitic infections and require extra caution when using antiparasitic medications.
Pregnant Women
- Safe options: Certain drugs like mebendazole or pyrantel pamoate may be used cautiously in later pregnancy for intestinal worms, but only under medical supervision.
- Unsafe or restricted drugs: Albendazole, ivermectin, and some antimalarials are generally avoided during the first trimester due to potential harm to the fetus.
- Prevention focus: For pregnant women, prevention through food safety, clean water, mosquito nets, and good hygiene is especially critical.
Children
- Dosage safety: Pediatric dosing is weight- and age-dependent. Medications like albendazole, mebendazole, and pyrantel pamoate are commonly prescribed for pinworms, roundworms, and hookworms.
- Common infections: Pinworms are the most frequent parasite in U.S. children, often causing nighttime anal itching and sleep disturbance.
- Extra care: Always consult a pediatrician before giving antiparasitics, as some drugs are not approved for children under 2 years.
Immunocompromised Individuals
- Higher risk: People with HIV/AIDS, those undergoing chemotherapy, or transplant patients may suffer more severe or chronic parasitic infections.
- Treatment challenges: They may require longer or combination therapy to fully clear parasites like Toxoplasma gondii or Cryptosporidium.
- Prevention priority: Safe food, water, and avoidance of high-risk exposures (e.g., raw meat, untreated water, cat litter for toxoplasmosis) are essential.
Global Health & Accessibility of Treatment
Despite effective antiparasitic drugs, parasites continue to cause a significant health burden worldwide, especially in low- and middle-income countries. Accessibility and affordability play a major role in treatment outcomes.
Why Parasites Remain a Global Burden
- Developing countries face higher rates of intestinal worms, malaria, and protozoan infections due to poor sanitation, limited access to clean water, and weak healthcare systems.
- Neglected tropical diseases (NTDs) such as schistosomiasis, lymphatic filariasis, and river blindness continue to affect millions despite being preventable.
- Travel and migration also spread parasites beyond endemic regions, making them a global concern.
Cost and Access Challenges
- In the United States, most antiparasitic medications like albendazole, ivermectin, or artemisinin-based therapies require a prescription and can be expensive without insurance.
- In resource-limited settings, these same drugs may be donated through global health initiatives, but shortages and delays in distribution are common.
- Access to diagnostic tools (stool tests, blood tests, imaging) is another barrier that delays proper treatment.
The Problem of Counterfeit Medications
- In some regions, counterfeit or substandard antiparasitic drugs circulate in local markets.
- These fake medicines may contain too little or no active ingredient, leading to treatment failure and drug resistance.
- Patients should only obtain medications from reliable pharmacies or healthcare providers to avoid harmful or ineffective products.
Future of Parasite Control
The fight against human parasites isn’t standing still. While current treatments save millions of lives each year, researchers are pushing boundaries to make parasite control more effective, safer, and accessible worldwide.
- Tackling Drug Resistance
- Just like bacteria, many parasites are developing resistance to existing drugs such as albendazole, ivermectin, and antimalarials.
- Ongoing research focuses on novel drug classes that work through different mechanisms, aiming to outsmart resistant strains.
- Combination therapies, already successful in malaria treatment, are being studied for other parasitic infections as well.
- Role of Vaccines
- A huge breakthrough in recent years has been the development of malaria vaccines (e.g., RTS,S and R21/Matrix-M). These represent major progress in reducing childhood deaths in endemic regions.
- Scientists are also investigating vaccines for hookworm, schistosomiasis, and leishmaniasis, which could dramatically cut global infection rates if proven effective.
- Advanced Diagnostics
- AI-powered tools are transforming parasite detection, helping laboratories identify infections more quickly and accurately.
- Molecular diagnostics (like PCR and next-gen sequencing) allow doctors to spot low-level infections and differentiate between parasite species—something traditional tests often miss.
- Point-of-care diagnostic kits are being designed for resource-limited settings, ensuring faster treatment and less transmission.
- The Big Picture
- Future control strategies will likely combine medications, vaccines, technology, and public health programs.
- The ultimate goal is not just treating infections, but reducing global parasite prevalence through prevention, early detection, and innovation.
Conclusion & Key Takeaways
Parasites in humans may sound frightening, but the good news is they are treatable with the right approach. Success depends on accurate diagnosis, choosing the correct medication, and following safe treatment practices.
Key reminders:
- Early detection matters – don’t ignore persistent digestive issues, unexplained fatigue, or skin/eye problems.
- Treatment works best under medical guidance – self-medicating can be dangerous and may lead to drug resistance.
- Prevention is powerful – good hygiene, safe food and water, and travel precautions can drastically lower your risk.
FAQs
1. What is the best treatment for parasites in humans?
The “best” treatment for human parasites is antiparasitic medication prescribed by a healthcare professional, as the specific drug and duration depend on the type and severity of the parasitic infection. Examples include anthelmintics for worms (like mebendazole or albendazole), antiprotozoal agents for single-celled parasites (like metronidazole), and ectoparasiticides for things like lice. While some infections can be resolved with a single dose, others require longer courses of treatment.
2. How do you know if your body is full of parasites?
If you continue to experience symptoms like stomach cramps and pain, nausea or vomiting, dehydration, weight loss, and digestive problems, including unexplained constipation, diarrhea, or persistent gas even after trying several treatments, you may have a parasite.
3. Can parasites cause fever?
Yes, parasites can cause fever, which may occur with the initial infection or a chronic one. Examples of parasitic infections that can cause fever include malaria, toxoplasmosis, schistosomiasis, and certain roundworm infections. Other common symptoms associated with parasitic infections, in addition to fever, can include abdominal pain, diarrhea, muscle aches, and fatigue.
4. Can parasites cause hives?
Yes, parasites can cause hives and other skin issues. Intestinal parasites can trigger an immune response, leading to the release of immunoglobulin E (IgE) and subsequent allergic reactions, including hives, rashes, and itching. Chronic itching, hives that don’t respond to treatment, or unexplained skin problems, especially with a history of travel abroad or unexplained high levels of eosinophils in the blood, may indicate a parasitic infection and should be evaluated by a doctor.
5.How do I check myself for parasites?
To check for parasites, a doctor should be consulted if you experience symptoms like diarrhea, bloating, weight loss, or fatigue. They can perform a stool test to look for eggs or parasite parts, or a tape test for pinworms by collecting eggs from the anal area. Other tests, such as blood tests, imaging tests, and colonoscopies, may be used to diagnose the specific type and extent of the infection.