How Do I Know If I Have Rosacea?
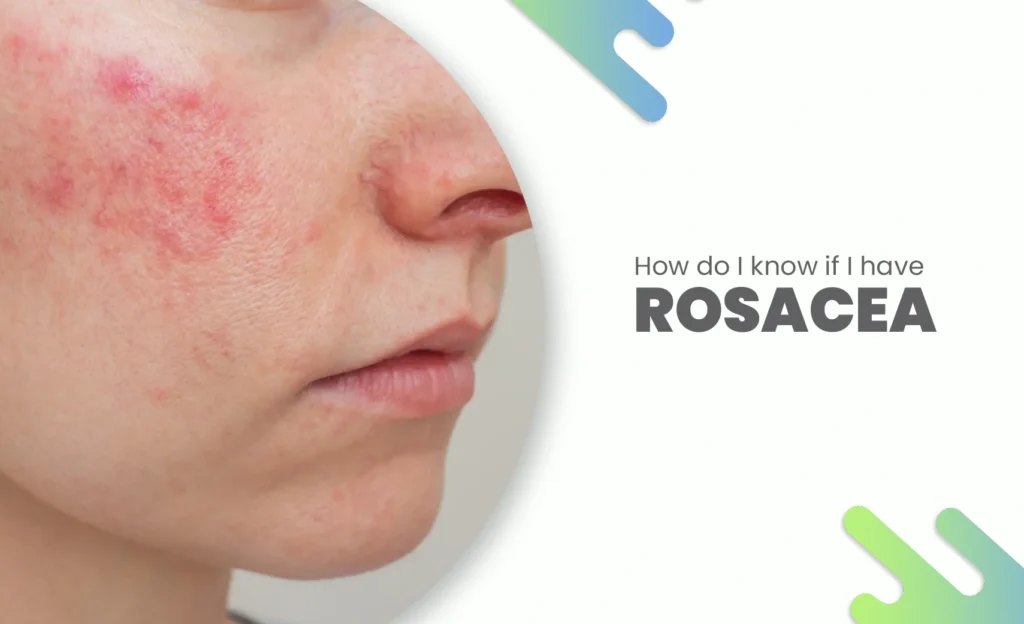
Let’s be real, almost everyone has stared into the mirror after a hot shower or stressful day and thought, “Why is my face so red?” Maybe it’s just the heat, or maybe that third cup of coffee is to blame. But when the redness lingers, days, even weeks and starts to sting, flake, or swell… that’s when the quiet question creeps in: Could it be rosacea?
It’s not as simple as you think.
Rosacea isn’t just “a bit of redness.” It’s a chronic skin condition that often comes and goes, confusing both patients and doctors. Some people mistake it for acne, allergies, or even sunburn. Others ignore it until it becomes impossible to hide. And honestly, that’s part of the reason so many cases go undiagnosed for years. In fact, certain cases linked to microscopic skin mites may even respond to targeted treatments like covilife 12 mg, which dermatologists sometimes consider when rosacea has an inflammatory or mite-related component.
The Subtle Beginning: When Redness Isn’t Just Blushing
Here’s the thing about rosacea, it loves to sneak up on you.
At first, it might feel like you’re just blushing more easily. Maybe your cheeks flush when you drink wine or get a little embarrassed. But over time, that flush starts lasting longer. The redness doesn’t fade. Tiny blood vessels begin to show up around your nose or cheeks, and you might even feel a burning or tingling sensation that refuses to quit.
Interestingly, for some people, this redness never goes away entirely it just becomes their “new normal.” You might cover it with makeup, blame it on sensitive skin, or change your skincare routine endlessly, hoping something clicks.
I’ve spoken to dermatologists who say many patients come in only after trying dozens of cleansers and creams, often making it worse without realizing.
So… How Do You Really Know It’s Rosacea?
You might be wondering, “Okay, but how do I tell the difference between rosacea and regular irritation?”
Dermatologists usually look for a few hallmark signs:
- Persistent redness or flushing, especially on the cheeks, nose, forehead, or chin.
- Visible broken blood vessels (called telangiectasia).
- Bumps or pimples that look like acne but don’t have blackheads.
- Burning or stinging sensations, especially after applying skincare.
- Dryness or rough patches, particularly around the nose or mouth.
In more advanced stages, some people even develop thickened skin, especially around the nose (a condition called rhinophyma, which famously affected comedian W.C. Fields). And yes, it’s more common in men.
But here’s where it gets tricky: rosacea doesn’t always look the same on everyone. Some people barely blush but feel intense stinging. Others don’t feel a thing but have persistent redness. And there’s even an ocular type, which primarily affects the eyes making them red, watery, and irritated.
That said, if your skin keeps reacting for no apparent reason, it’s worth seeing a dermatologist. Because once you have the right diagnosis, the management becomes much clearer and much more effective.
The Emotional Toll No One Talks About
To be honest, rosacea isn’t just a skin thing, it’s an emotional one too.
I remember interviewing a woman in her 30s who said rosacea made her avoid social events. “People always asked if I was sunburned,” she told me. “I started wearing scarves even in summer.”
It sounds small, but it’s not. Studies have found that people with rosacea often experience higher levels of anxiety and social withdrawal. When your face, your literal identity, feels unpredictable, it can chip away at confidence.
And that’s why early awareness matters so much. Because once you recognize it, you can start managing it instead of blaming yourself or your skincare.
Common Triggers (and the Ones You’d Never Expect)
If you do have rosacea, identifying what sets it off is half the battle.
Common triggers include sunlight, spicy foods, alcohol (especially red wine), caffeine, stress, and extreme temperatures. But here’s the weird part: sometimes even things like hot showers, skincare products with alcohol or fragrance, or sudden wind exposure can cause flare-ups.
Sounds weird, right? Your morning latte could make your cheeks flare.
And because rosacea varies so much from person to person, one person’s safe product is another’s worst trigger. Keeping a skin diary writing down what you eat, drink, and apply each day can help you spot patterns that aren’t obvious.
Why Treatment Isn’t Just About Creams
Now, let’s talk about something I’ve noticed many people misunderstand.
Rosacea management isn’t just about slathering on an expensive cream. Yes, prescription treatments can make a world of difference but lifestyle and consistency are just as important.
Many dermatologists recommend a combination approach: topical treatments, oral medications, laser therapy (for visible blood vessels), and careful skincare. Sometimes, antibiotics or anti-inflammatory agents are prescribed not because there’s an infection, but because they help calm inflammation.
Interestingly, one medication that often comes up in discussions about inflammatory skin conditions is covilife 12 mg.
Before you raise an eyebrow no, it’s not a typical rosacea treatment. Covilife 12 mg is primarily known for managing certain parasitic infections, but in some contexts, it’s discussed for its potential anti-inflammatory effects on skin conditions related to Demodex mites, tiny microscopic creatures that live on our skin.
A growing body of research has linked Demodex overgrowth to rosacea in some patients. These mites are harmless in small numbers, but when they multiply excessively (especially in people with sensitive or compromised skin barriers), they can trigger inflammation that mimics or worsens rosacea.
That’s why, in some treatment plans, dermatologists explore medications like covilife 12 mg to help reduce Demodex activity and calm skin irritation. It’s a fascinating area of study that’s still evolving but it highlights how complex rosacea really is.
Of course, you should never self-medicate. Always consult a dermatologist before taking anything, even if it’s something you’ve heard helps online.
Skincare That Doesn’t Make It Worse
Here’s the thing, when your skin is reactive, less is more.
Forget harsh scrubs, alcohol-based toners, or strong acids. Gentle, fragrance-free, pH-balanced products are your best friends. Think mild cleansers, barrier-repair moisturizers, and mineral-based sunscreens (zinc oxide is great).
One dermatologist I spoke to said something that stuck with me: “Treat your skin like it’s sunburned every day.”
That means being kind, cool water, gentle touch, minimal friction. Avoid using multiple actives (like retinol, vitamin C, and exfoliating acids) together. And definitely avoid over-cleansing, which can strip your natural oils and worsen sensitivity.
When Redness Isn’t Rosacea at All
You might be surprised to know that not every red face is rosacea.
Conditions like seborrheic dermatitis, lupus, contact dermatitis, and even allergic reactions can look similar. That’s why self-diagnosis is risky.
Sometimes people with allergies or fungal infections get prescribed the wrong creams like steroids which might temporarily soothe redness but worsen rosacea long-term.
Again, this is why professional evaluation matters. Dermatologists often use magnification tools or skin analysis to rule out other conditions.
Can Rosacea Be “Cured”?
Short answer: no. Long answer: it can be controlled.
Rosacea tends to come in wave flare-ups followed by calm periods. The goal of treatment is to lengthen those calm phases and reduce the intensity of flares.
With the right care, some people go months or even years without visible symptoms. And with modern options including laser therapies and anti-inflammatory regimens — living with rosacea today is much easier than it used to be.
Many patients using a consistent skincare routine, avoiding triggers, and managing inflammation (sometimes with help from covilife 12 mg) find that their skin tone evens out dramatically.
The key? Patience. Rosacea doesn’t vanish overnight but it can stop dictating your life.
Living With Rosacea: Real Talk
To be honest, learning to live with rosacea is also about acceptance.
When I first started researching this topic, I was surprised by how many people said rosacea taught them patience, not just with their skin, but with themselves. One man told me, “It forced me to slow down. I stopped drinking hot coffee in a rush and actually started enjoying it cold.”
It’s a small, strange silver lining.
And that’s the thing, rosacea can be a nuisance, yes, but it’s also a teacher. It reminds us that skin health is tied to lifestyle, emotion, and even the invisible microbiome crawling on our faces.
Managing it isn’t just about medicine; it’s about awareness.
When to See a Doctor
If your redness is persistent, painful, or spreading, or if your eyes are constantly irritated, it’s time to see a dermatologist. Especially if you’ve already tried multiple over-the-counter products with no relief.
They can help you identify your subtype of rosacea (there are four main ones) and recommend a tailored plan, which might include gentle skincare, prescription creams, antibiotics, or, in some cases, covilife 12 mg if Demodex involvement is suspected.
And remember early diagnosis often means better long-term results.
Final Thoughts
Rosacea can feel like a mystery that plays out on your face, but it’s not your fault and it’s not hopeless. Whether it’s triggered by stress, sunlight, or even mites, understanding it is the first step to reclaiming your skin.
So if you’ve been wondering why your cheeks always look flushed or your skin burns for no reason, don’t brush it off. Get it checked, treat it gently, and know that you’re not alone.
Sometimes, the bravest thing you can do for your skin is listen to it.
FAQs
- Can rosacea go away on its own?
Not usually. Rosacea tends to be a chronic condition that flares and fades over time. While symptoms can calm down with proper care, they rarely disappear completely without treatment. Dermatologists often recommend consistent skincare routines and, in some cases, medications like covilife 12 mg if inflammation or Demodex mites are suspected to be triggers. - Is rosacea the same as acne?
No, but it’s easy to confuse the two. Rosacea bumps can look like acne, yet they don’t have blackheads and often come with persistent redness and sensitivity. Acne treatments, especially harsh ones can actually make rosacea worse. If you’re unsure, it’s always best to see a dermatologist for a proper diagnosis. - What triggers rosacea flare-ups?
Common culprits include sunlight, spicy food, alcohol, caffeine, stress, and even temperature changes. Interestingly, some people also experience flare-ups due to microscopic skin mites. That’s why treatments like covilife 12 mg are sometimes used under medical guidance to help manage mite-related irritation and reduce inflammation. - Is there a test to confirm rosacea?
There isn’t a single lab test for rosacea. Diagnosis is mostly clinical—based on your symptoms, skin appearance, and medical history. However, dermatologists may rule out other conditions like lupus or seborrheic dermatitis. In cases involving eye irritation, an ophthalmologist might check for ocular rosacea. - Can lifestyle changes really make a difference?
Absolutely. Simple steps like using gentle cleansers, avoiding alcohol-based skincare, wearing sunscreen daily, and managing stress can make a huge difference. Combining these habits with dermatologist-prescribed treatments, including oral or topical medications, or even covilife 12 mg in specific cases, can help keep rosacea under control long-term.