Demodex Mites on Humans: Are They Harming Your Skin?

What are Demodex Mites?
Demodex mites are microscopic parasites that naturally live on human skin, especially in areas rich in sebaceous (oil) glands such as the face, eyelids, and scalp. Almost every adult carries them in small numbers, but when their population grows excessively, it can lead to skin irritation, inflammation, or conditions like rosacea and blepharitis. Presence of Demodex Mites on Humans is usually harmless, as they normally feed on dead skin cells and skin oils, but under certain conditions, like a weakened immune system, oily skin, or poor hygiene, they can cause a Demodex infestation (demodicosis).
Anatomy of Demodex Mites
Demodex mites have a distinctive worm-like body, perfectly adapted to living inside hair follicles and sebaceous glands.
- Size: Around 0.2–0.4 mm long, invisible to the naked eye and only seen under a microscope.
- Body structure: Divided into two main segments – the gnathosoma (mouthpart) and the opisthosoma (elongated abdomen).
- Legs: Each mite has four short pairs of legs near the head, which they use to cling to follicles and crawl slowly.
- Color & texture: Semi-transparent, making them difficult to detect without lab tests.
- Adaptations: Their elongated body allows them to bury deep inside follicles, while claw-like structures help them hold onto the skin.
Life Cycle of Demodex Mites
The life of a Demodex mite is short but rapid, usually lasting two to three weeks.
- Egg stage – Female mites lay eggs inside hair follicles or sebaceous glands.
- Larvae stage – Eggs hatch into six-legged larvae within a few days.
- Nymph stage – The larvae molt into nymphs, developing eight legs.
- Adult stage – Adults reach maturity in about 7 days and continue mating within follicles.
- Death & decomposition – After mating, mites die inside the follicle, where their bodies disintegrate, potentially contributing to inflammation or skin irritation.
Because of this rapid cycle, infestations can escalate quickly if conditions allow uncontrolled growth.
Types of Demodex Mites
There are two main species of Demodex mites that infest humans:
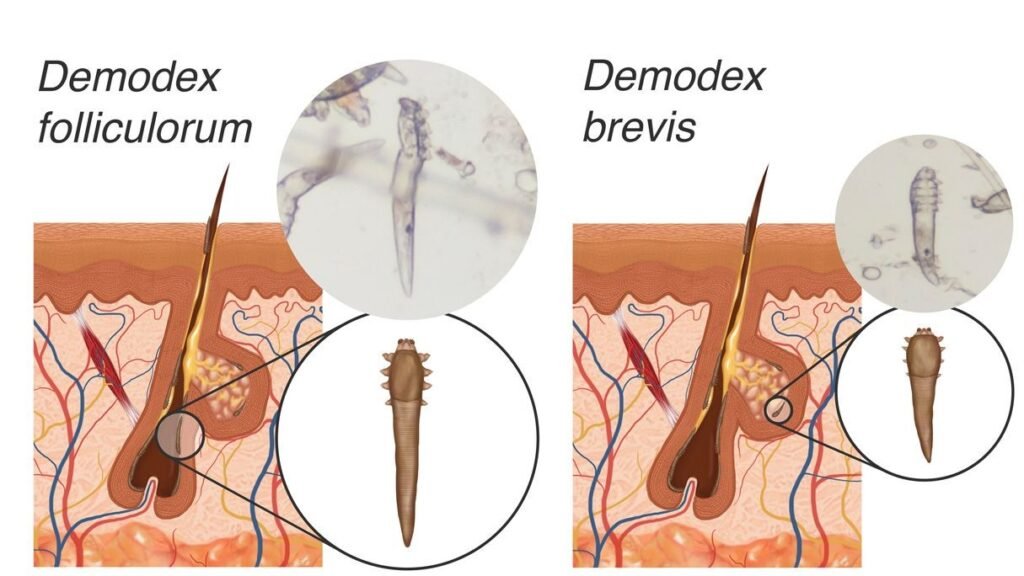
- Demodex folliculorum
- Lives primarily in hair follicles, especially on the face (nose, cheeks, forehead).
- Feeds on skin cells and oils.
- More strongly linked with rosacea, enlarged pores, and rough skin texture.
- Demodex brevis
- Burrows deeper into the sebaceous glands attached to hair follicles.
- Feeds mainly on sebum (skin oil).
- More commonly associated with seborrheic dermatitis, oily skin issues, and blocked glands.
Both types can coexist on human skin, and together, they form the Demodex population that may remain harmless or trigger skin problems when overgrown.
Demodex and Human Interaction
Demodex mites are permanent companions of humans. In fact, studies show that nearly 80–90% of adults have these mites living on their skin, often without any visible symptoms. They are most commonly found on the face, scalp, ears, and eyelids, areas rich in oil-producing sebaceous glands.
For the most part, these tiny organisms go unnoticed. They help clean up excess oils and dead skin cells, quietly existing in balance with our skin’s natural ecosystem. Problems arise when the balance shifts, leading to itching, redness, bumps, or eye irritation. This delicate interaction makes Demodex mites both harmless inhabitants and potential troublemakers depending on the situation.
Symbiotic Relationship with Humans
The relationship between Demodex mites and humans is often described as commensal or mildly symbiotic:
- Normal role: They consume skin oils (sebum) and shed cells, preventing excess buildup in follicles.
- Neutral presence: Most people never realize they carry them, since the immune system usually keeps their numbers under control.
- Microbiome connection: Some researchers suggest that Demodex mites play a role in maintaining the skin microbiome balance, much like certain bacteria in our gut.
In short, having Demodex is normal and natural. It’s not their presence that’s harmful, it’s their overpopulation that can tip the scale from symbiosis to skin disease.
Conditions Leading to Demodicosis
Demodicosis is the medical term for skin problems caused by an overgrowth of Demodex mites. While everyone has them, only some people develop this condition. Factors that increase the risk include:
- Weakened immune system – Conditions like HIV, cancer, or long-term steroid use reduce the body’s ability to control mite populations.
- Excess oily skin – High sebum production provides an abundant food source for mites.
- Skin disorders – People with rosacea, seborrheic dermatitis, or chronic blepharitis are more prone.
- Aging – Elderly individuals tend to have higher mite counts due to oil gland changes.
- Stress and hormonal imbalance – These can trigger increased oil production and flare-ups.
- Poor skin hygiene – Irregular cleansing may allow mites to multiply unchecked.
When these conditions align, mite populations explode, leading to redness, itching, pustules, eyelid irritation, or worsening of rosacea symptoms.
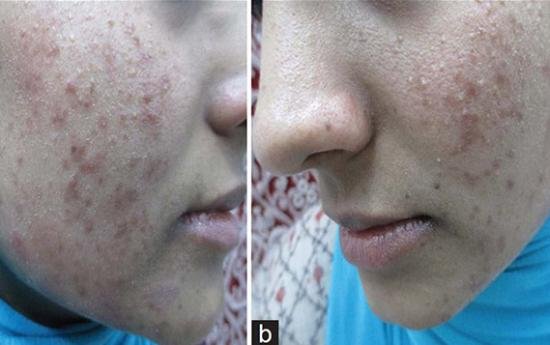
Identifying Demodex-Related Symptoms
Most people carry Demodex mites without ever noticing them. But when their numbers rise beyond normal, they trigger visible skin and eye symptoms. Identifying these signs early is crucial because mite overgrowth is often mistaken for acne, rosacea, or simple skin irritation. Unlike typical breakouts, Demodex-related symptoms usually appear in clusters around the nose, cheeks, forehead, eyelashes, and scalp.
Common Symptoms of Infestation
An overgrowth of Demodex mites can lead to:
- Persistent itching – Especially at night when mites are more active.
- Redness and inflammation – Often misdiagnosed as rosacea or eczema.
- Pimples or pustules – Acne-like eruptions that don’t respond to standard acne treatments.
- Crawling sensation – A subtle feeling of something moving under the skin.
- Scaly or rough patches – Caused by excessive skin cell buildup.
- Hair thinning – In some cases, mites can affect scalp follicles.
These symptoms tend to flare up in oily areas like the T-zone of the face, where mites find abundant sebum to feed on.
Recognizing Demodex Folliculitis
When mites excessively invade hair follicles, the condition is called Demodex folliculitis. It presents as:
- Small red bumps or pustules around hair follicles.
- Clusters of breakouts that resemble acne but don’t clear with typical acne treatments.
- Increased skin sensitivity – burning or stinging when applying skincare products.
- Localized hair loss – due to follicle inflammation and blockage.
Unlike bacterial folliculitis, Demodex folliculitis is not caused by infection, but by mite-induced irritation and inflammation.
Eye-Related Issues and Symptoms
Demodex mites also infest eyelashes and eyelids, leading to a condition known as Demodex blepharitis. Symptoms include:
- Itchy or burning eyelids – often worse in the morning.
- Red, inflamed eyelid margins – making eyes appear tired or irritated.
- Crusty flakes at the base of eyelashes – sometimes mistaken for dandruff.
- Loss or misdirection of eyelashes – due to follicle damage.
- Dry eyes or watery eyes – from disrupted tear gland function.
- Recurrent styes or chalazia – caused by blocked oil glands in the eyelid.
Because eye symptoms are so specific, ophthalmologists often check for Demodex mites under the microscope when patients present with chronic blepharitis that doesn’t improve with standard care.
Diagnosing Demodicosis
Because Demodex mites are microscopic and live deep inside hair follicles and sebaceous glands, diagnosing demodicosis (mite overgrowth) can be tricky. Many of the symptoms – like acne-like bumps, redness, or eyelid irritation, overlap with other skin conditions such as rosacea, eczema, or bacterial folliculitis. That’s why proper diagnosis is essential to confirm whether Demodex mites are truly the underlying cause.
Medical Diagnosis Techniques
Dermatologists and ophthalmologists use a few reliable methods to detect Demodex:
- Skin Scraping Test – A small scraping of skin is taken and examined under a microscope to check for mites, eggs, or larvae.
- Adhesive Tape Test – Clear tape is pressed on the skin, removed, and then examined under a microscope to count mites.
- Cylindrical Dandruff Check (Eyelashes) – Crusty debris at the base of eyelashes is examined, often revealing Demodex mites linked to blepharitis.
- Standardized Skin Surface Biopsy (SSSB) – A layer of skin with sebaceous secretions is removed to measure mite density per square centimeter.
- Microscopy Examination – Doctors directly look for moving mites, which confirms infestation.
These methods help determine not only the presence of mites but also the density, which is crucial since low numbers are normal and only high populations indicate infestation.
Self-Check Methods
While a professional exam is the most reliable way to confirm demodicosis, certain signs at home can raise suspicion:
- Persistent symptoms – If breakouts or redness don’t respond to acne or rosacea treatments, mites may be the hidden cause.
- Crawling or itching at night – Mites are most active in the dark, so worsening nighttime itching is a common clue.
- Eyelid debris – Crusty flakes at the base of eyelashes, especially in the morning, can point to Demodex blepharitis.
- Patchy irritation in oily zones – Breakouts centered around the nose, forehead, or chin often suggest mite activity.
However, self-checks cannot confirm Demodex with certainty. Since symptoms mimic many other conditions, a dermatologist or eye specialist should always be consulted for accurate testing.
Treatment and Management of Demodicosis
When Demodex mites multiply excessively and trigger skin or eye problems, the condition is known as demodicosis. The good news is, it can be managed with a combination of medical treatments, natural remedies, and preventive care. The key is not just killing the mites but also reducing the conditions that allow them to thrive.
Medical Treatments and Prescriptions
Dermatologists and ophthalmologists often prescribe targeted treatments to control mite populations and ease inflammation:
- Topical Ivermectin – A prescription cream or gel that directly kills Demodex mites and reduces skin irritation.
- Metronidazole Cream/Gel – Commonly used for rosacea, it also helps control mite-related inflammation.
- Permethrin Cream – An antiparasitic cream that eliminates mites and prevents reinfestation.
- Oral Ivermectin – Like Iverheal 6mg Prescribed for severe or widespread infestations.
- Antibiotics (oral or topical) – Used if bacterial infections develop from irritated skin.
- Lid Scrubs and Ophthalmic Ointments – For Demodex blepharitis, doctors may recommend medicated eyelid cleansers or ointments.
⚠️ Medical treatment should always be guided by a healthcare professional since dosage and duration vary based on severity.
Home Remedies and Natural Solutions
For mild cases or as supportive care alongside prescriptions, some natural approaches can help reduce mite activity:
- Tea Tree Oil – Widely studied for its ability to kill Demodex mites, especially in eyelid scrubs and diluted skincare solutions.
- Neem Oil – Known for its antibacterial and antiparasitic properties.
- Aloe Vera – Soothes redness and irritation caused by mite activity.
- Washing Bedding in Hot Water – Helps eliminate mites from pillowcases and sheets.
- Gentle Daily Cleansing – Removes excess sebum, reducing mite food supply.
- Avoiding Oily Skincare – Oil-rich products may worsen infestations.
⚠️ Tea tree oil must be diluted before use, especially around the eyes, to prevent irritation.
Preventive Measures for Reducing Risk
Since Demodex mites are part of our natural skin ecosystem, complete elimination is impossible, and unnecessary. Prevention focuses on keeping their population in check:
- Maintain Good Skin Hygiene – Regular cleansing helps remove sebum and dead skin cells.
- Use Non-Comedogenic Products – Choose oil-free skincare to reduce mite-friendly environments.
- Replace or Wash Pillowcases Often – Prevents reinfestation, especially in eye-related cases.
- Manage Underlying Skin Conditions – Treating rosacea, seborrheic dermatitis, or oily skin lowers risk.
- Boost Immune Health – A healthy immune system naturally keeps mite populations balanced.
- Limit Stress and Fatigue – Stress hormones can increase oil production, creating conditions for mites to thrive.
By combining medical care, natural remedies, and prevention, most people can successfully control demodicosis and restore healthy skin and eye comfort.
Demodex Mites and Eye Health
While Demodex mites are mostly associated with facial skin, they are also a major culprit behind chronic eye problems. These mites often infest the eyelash follicles and sebaceous glands of the eyelids, leading to irritation and inflammation. In fact, studies suggest that Demodex blepharitis (inflammation of the eyelids caused by mites) is one of the most underdiagnosed eye conditions worldwide.
Understanding Their Impact on Eye Conditions
When Demodex mites multiply on the eyelids and lashes, they disrupt the delicate balance of the eye’s protective barrier. This can lead to:
- Blepharitis – Red, swollen, and itchy eyelids often accompanied by crusty flakes at the lash line.
- Dry Eye Syndrome – Mites block the meibomian glands (oil glands in the eyelids), reducing tear film quality and causing dryness.
- Recurrent Styes and Chalazia – Blocked oil glands from mite buildup trigger painful lumps on the eyelid.
- Eyelash Loss or Misalignment – Follicle damage may cause lashes to fall out or grow in abnormal directions.
- Ocular Rosacea – Mite overgrowth may worsen rosacea-related eye symptoms like redness and burning.
Because these symptoms often mimic other eye conditions, Demodex is frequently overlooked as the root cause.
Treatment and Management for Eye-Related Issues
Managing Demodex-related eye conditions involves reducing mite populations while soothing irritation:
- Tea Tree Oil Eyelid Scrubs – Specialized wipes or cleansers with diluted tea tree oil effectively kill mites and remove debris.
- Warm Compresses – Helps unclog blocked oil glands and improve tear flow.
- Lid Hygiene Routine – Regular cleaning with medicated eyelid cleansers is essential for long-term control.
- Topical or Oral Ivermectin – In stubborn cases, doctors may prescribe antiparasitic medications.
- Artificial Tears – Provide relief from dryness caused by gland dysfunction.
- Antibiotic or Steroid Drops (if prescribed) – Used for secondary bacterial infections or severe inflammation.
Early treatment is key, since untreated Demodex blepharitis can become chronic and recurrent, leading to ongoing eye discomfort. A consultation with an ophthalmologist is recommended for accurate diagnosis and tailored therapy.
Living with Demodex Mites
Since Demodex mites are a natural part of human skin, the goal isn’t to eliminate them completely, it’s about keeping their numbers under control. Most people live with these mites without any issues, but for those prone to flare-ups, a few adjustments in daily habits can make living with them much easier.
Tips for Comfortable Coexistence
- Keep Skin Clean, Not Stripped – Wash your face daily with a gentle, non-oily cleanser to remove excess sebum without irritating the skin.
- Stick to Non-Comedogenic Products – Choose oil-free makeup and skincare so you’re not “feeding” the mites.
- Practice Eyelid Hygiene – If you’re prone to eye irritation, use lid scrubs or medicated wipes regularly.
- Change Pillowcases Often – Wash them in hot water at least twice a week to avoid reinfestation.
- Manage Stress – High stress can trigger flare-ups by increasing oil production and lowering immunity.
- Avoid Overusing Harsh Products – Excess exfoliation or strong chemicals can weaken the skin barrier, making it easier for mites to thrive.
These small lifestyle changes help maintain a healthy balance between skin and mites, minimizing discomfort.
Importance of Long-term Care and Maintenance
Demodex infestations tend to recur if long-term care is ignored. Since mites are part of your skin ecosystem, treatment should be viewed as ongoing management rather than a one-time fix. Long-term strategies include:
- Regular Dermatologist Checkups – Especially if you struggle with rosacea, blepharitis, or recurring skin irritation.
- Consistent Hygiene Routine – Even after symptoms improve, maintaining eyelid and skin cleansing prevents future overgrowth.
- Supporting Skin Barrier Health – Hydrating moisturizers and a balanced diet rich in antioxidants help your skin defend against flare-ups.
- Immune System Support – Good sleep, stress control, and a nutrient-rich diet strengthen your natural defenses.
With proper maintenance, most people can keep Demodex mites harmless cohabitants instead of problematic pests.
Expert Insights and Professional Advice
When it comes to Demodex mites, there’s a lot of misinformation floating around online. While home remedies and over-the-counter solutions can help, professional medical guidance is often the most reliable way to manage persistent symptoms. Dermatologists and eye specialists can provide personalized treatment plans and ensure that what you’re experiencing is truly related to Demodex, not another skin or eye condition.
Consulting Dermatologists and Healthcare Providers
- Dermatologists can run tests like skin scrapings or biopsies to confirm mite overgrowth and recommend treatments such as ivermectin, metronidazole, or permethrin.
- Ophthalmologists can diagnose Demodex blepharitis by examining eyelashes and meibomian glands, then suggest targeted lid hygiene routines or medicated wipes.
- Primary Care Providers may also help rule out other underlying conditions that mimic Demodex symptoms, such as bacterial infections or allergies.
Seeking professional advice ensures you’re not misdiagnosing yourself and wasting time on ineffective treatments.
Utilizing Reliable Information Sources
Since Demodex mites are a complex and sometimes controversial topic, it’s important to rely on trusted, evidence-based resources:
- Peer-Reviewed Medical Journals – Research on Demodex and skin microbiome continues to evolve.
- Dermatology and Ophthalmology Associations – Websites from organizations like the American Academy of Dermatology (AAD) or American Academy of Ophthalmology (AAO) provide accurate, updated guidance.
- Hospital and University Websites – Mayo Clinic, Cleveland Clinic, and academic dermatology departments often publish reliable patient information.
- Licensed Professionals – Online forums and DIY groups may spread myths; always verify with a certified healthcare provider.
By combining expert medical care with credible information sources, you can confidently manage Demodex mites without falling into the trap of misinformation.
FAQs
Q1. Are there different types of Demodex mites?
Yes. The two main species that affect humans are Demodex folliculorum, which lives in hair follicles, and Demodex brevis, which inhabits sebaceous (oil) glands.
Q2. What do Demodex mites look like?
They are microscopic, cigar-shaped mites measuring about 0.1–0.4 mm long, with a semi-transparent body and tiny legs near the head.
Q3. How common is demodicosis?
Very common. Studies suggest that over 80% of adults carry Demodex mites, but only a small fraction develop symptomatic infestation (demodicosis).
Q4. What are the symptoms of Demodex folliculitis?
Typical symptoms include itchy or burning skin, red bumps, pustules, scaling, and a crawling sensation, often on the face, scalp, or chest.
Q5. Are Demodex mites contagious?
Yes, but only mildly. They can spread through close skin-to-skin contact or sharing items like towels and bedding, though most people already harbor them naturally.
Q6. How is Demodex folliculitis diagnosed?
Dermatologists usually confirm it with skin scrapings, biopsies, or microscopic examination to detect mites, eggs, or waste material.
Q7. How is demodicosis treated?
Treatment may include topical or oral medications such as ivermectin, permethrin, benzyl benzoate, or tea tree oil formulations, often combined with gentle skin care.
Q8. What can I expect if I have demodicosis?
With proper treatment, symptoms typically improve within 4–6 weeks, though relapses can occur if underlying triggers (like oily skin or weak immunity) persist.
Q9. How can I reduce my risk of demodicosis?
Maintain good facial hygiene, avoid oily skincare products, wash bedding regularly, and manage stress or chronic skin conditions that may worsen mite overgrowth.
Q10. How do I get rid of face mites at home?
Mild cases may improve with tea tree oil cleansers, lid scrubs for eyelashes, and non-comedogenic skincare, but persistent symptoms require medical treatment.
References:
- Paichitrojjana, A., & Chalermchai, T. (2024). Evaluating the Efficacy of Oral Ivermectin on Clinical Symptoms and Demodex Densities in Patients with Demodicosis. Drug design, development and therapy, 18, 5299–5306. https://doi.org/10.2147/DDDT.S498938
- Smith, M., Wolffsohn, J. S., & Chiang, J. C. B. (2024). Topical ivermectin 1.0% cream in the treatment of ocular demodicosis. Contact lens & anterior eye : the journal of the British Contact Lens Association, 47(1), 102099. https://doi.org/10.1016/j.clae.2023.102099
- de Rojas, M., Riazzo, C., Callejón, R., Guevara, D., & Cutillas, C. (2012). Morphobiometrical and molecular study of two populations of Demodex folliculorum from humans. Parasitology research, 110(1), 227–233. https://doi.org/10.1007/s00436-011-2476-3 |
- Kubanov, A., Gallyamova, Y., & Kravchenko, A. (2019). Clinical picture, diagnosis and treatment of rosacea, complicated by Demodex mites. Dermatology reports, 11(1), 7675. https://doi.org/10.4081/dr.2019.7675