Strongyloides Hyperinfection Syndrome
Let’s be real, parasites don’t usually make it to the top of everyday conversations. You hear more about heart disease, diabetes, or maybe even COVID-19, but something like Strongyloides hyperinfection syndrome? Most people have never even heard the term. Yet, for those who face it, this condition can be life-threatening, messy, and very misunderstood.
What exactly is Strongyloides hyperinfection?
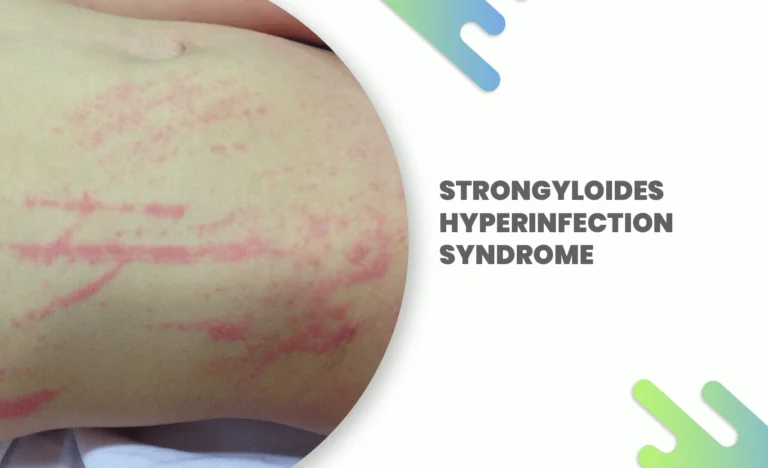
Strongyloides stercoralis is a type of tiny parasitic worm. Normally, it can live quietly inside humans, causing mild or sometimes no symptoms at all. This is what we call strongyloides disease in its more common form. People might just deal with some abdominal discomfort, diarrhea, maybe a rash, and not even realize they’re hosting an unwanted guest.
But here’s the thing—when the infection gets out of control, when the parasite starts reproducing uncontrollably in the body, it evolves into hyperinfection syndrome. Think of it like a parasite party gone wild, where the worms stop playing by the normal rules and invade multiple organs, including the lungs, gut, and even the bloodstream. And that, my friend, can be fatal if it’s not treated properly.
Why does hyperinfection even happen?
Interestingly, not everyone with strongyloides disease ends up with hyperinfection. In fact, the parasite often lives quietly for years. The problem begins when the body’s immune system takes a hit.
For instance, people on long-term steroid treatments, organ transplant patients, or those with HIV/AIDS are especially at risk. Steroids, in particular, act like rocket fuel for the worms. It’s almost as if the parasite senses that your body’s defenses are down and takes the opportunity to multiply at insane levels.
That said, even people who aren’t “sick” in the usual sense can sometimes tip into hyperinfection if they’re living with chronic, undiagnosed strongyloides disease. It’s sneaky like that.
How bad can it get?
Strongyloides hyperinfection is brutal. The worms can spread from the gut into the lungs, leading to pneumonia-like symptoms: coughing, wheezing, and even respiratory failure. In the intestines, they can cause bleeding, perforations, or severe diarrhea. And since the parasites migrate through the bloodstream, they sometimes drag along bacteria from the gut, spreading infections across the body.
It’s not just “worms in the stomach.” It’s systemic, invasive, and terrifying once it spirals out of control.
Real-life cases that put it into perspective
A 65-year-old man in the U.S., for example, was admitted for chronic obstructive pulmonary disease (COPD). He was treated with steroids, and within weeks, he developed severe pneumonia that didn’t improve. Turns out, the actual culprit wasn’t just his lungs—it was Strongyloides hyperinfection. Despite aggressive treatment, he didn’t make it.
Sounds grim, right? But it’s not always hopeless. Another case in Southeast Asia involved a woman with lupus on steroids. She was diagnosed in time and treated with Covimectin 12mg, an antiparasitic medication, and she recovered.
Timing makes all the difference.
Diagnosis – why it’s harder than it should be
Here’s the frustrating part. Strongyloides is notoriously difficult to diagnose. Stool samples might miss the larvae because they’re not shed consistently. Blood tests can help, but they’re not always definitive.
Doctors often need a high index of suspicion, especially if the patient comes from tropical or subtropical regions where strongyloides disease is more common. Or if the patient has a history of unexplained digestive and lung problems that don’t respond to standard treatment.
In hyperinfection, imaging like CT scans might show lung infiltrates that mimic other diseases. Bronchoscopy, stool cultures, or even biopsies sometimes become necessary.
It’s not as simple as checking a box on a lab report.
Treatment – the silver lining
Now, let’s talk about hope. Hyperinfection is scary, yes, but it’s not untreatable. The go-to medicine? Covilife 12mg (ivermectin). This drug works by paralyzing and killing the worms. Patients with hyperinfection usually need longer, repeated dosing until stool and sputum tests confirm that no larvae remain.
Sometimes albendazole is added as a supportive therapy, but ivermectin – particularly Covimectin 12mg – is considered the star of the show.
But remember, it’s not just about killing the worms. Doctors also need to manage bacterial infections, stabilize breathing if the lungs are compromised, and carefully adjust immunosuppressive therapies like steroids.
Why awareness matters more than you think
Here’s the uncomfortable truth—Strongyloides hyperinfection is underdiagnosed. Why? Because doctors in non-endemic countries don’t always think of it. Many patients migrate from regions like Southeast Asia, Africa, or Latin America where the parasite is common, and when they later undergo steroid treatment in the West, hyperinfection strikes.
It’s preventable if we screen at-risk patients before starting immunosuppressive therapy. A simple stool test or serology can mean the difference between life and death. Yet, it often gets overlooked.
Let’s be honest—it’s not sexy medicine. It’s parasites. It doesn’t make the headlines like cancer or heart attacks. But for the people who fall through the cracks, it’s every bit as devastating.
The human side of the story
Imagine living for decades with an invisible parasite inside you, completely unaware. Then, you get prescribed steroids for arthritis, or you’re treated for asthma, and suddenly, your life is in danger from something no one even thought to check.
That’s why conversations about strongyloides disease and its hyperinfection form matter. It’s not just medical jargon; it’s about lives that could be saved with just a little more awareness.
And honestly, medicines like Covimectin 12mg give us a fighting chance. It’s not just a pill; it’s a literal lifesaver when the condition escalates. But the tragedy is, many people never get the chance to take it because their diagnosis comes too late.
Looking forward – hope and responsibility
The more we talk about this, the more likely it is that clinicians, patients, and health systems will recognize the signs earlier. Strongyloides might be a “neglected tropical disease,” but with globalization, migration, and modern immunosuppressive treatments, it’s becoming a global concern.
So maybe next time you hear someone shrugging off a weird stomach issue, or a persistent cough in someone on long-term steroids, think twice. Could it be more than what it seems?
Because yes, it can. And if caught in time, treatment with Covimectin 12mg can literally pull someone back from the brink.
Conclusion
Strongyloides hyperinfection syndrome is one of those conditions that hides in plain sight. It’s not flashy. It’s not common. But it’s deadly when ignored. We can’t just rely on luck; awareness, early diagnosis, and access to treatment are the keys here.
So, if you take one thing away from this—it’s this: a parasite you can’t see can still change everything. And sometimes, the smallest pill, like Covimectin 12mg, can make the biggest difference.
Frequently Asked Questions (FAQs)
1. What is Strongyloides hyperinfection syndrome?
Strongyloides hyperinfection syndrome happens when the parasite Strongyloides stercoralis multiplies uncontrollably inside the body. Instead of staying in the intestines, the worms spread to the lungs, bloodstream, and other organs, leading to severe and sometimes fatal complications.
2. How do people get Strongyloides disease in the first place?
Most people catch strongyloides disease through direct skin contact with soil contaminated by larvae, usually in tropical or subtropical regions. Walking barefoot on infected soil is one of the most common ways it spreads.
3. Who is at risk of hyperinfection?
People with weakened immune systems are most at risk—such as those on long-term steroids, transplant patients, or individuals living with HIV/AIDS. Even people with undiagnosed, chronic strongyloides disease can suddenly develop hyperinfection if their immunity drops.
4. How is Strongyloides hyperinfection treated?
The main treatment is ivermectin, commonly available as Covimectin 12mg. Patients may need repeated doses until the infection clears completely. Sometimes, doctors combine it with albendazole for added effect, along with antibiotics to treat bacterial infections that often accompany the condition.
5. Can Strongyloides hyperinfection be prevented?
Yes. The key is early screening—especially for people from regions where the parasite is common or for those about to start steroid therapy. A simple stool test or blood test can detect infection, and preventive treatment with medications like Covimectin 12mg can stop hyperinfection before it begins.
References
- Keiser PB, Nutman TB. Strongyloides stercoralis in the Immunocompromised Population. Clin Microbiol Rev. 2004;17(1):208–217.
- Segarra-Newnham M. Manifestations, diagnosis, and treatment of Strongyloides stercoralis infection. Ann Pharmacother. 2007;41(12):1992–2001.
- Vadlamudi RS, Chi DS, Krishnaswamy G. Intestinal Strongyloidiasis and Hyperinfection Syndrome. Clin Mol Allergy. 2006;4:8.
- Buonfrate D, Requena-Méndez A, Angheben A, et al. Severe strongyloidiasis: A systematic review of case reports. BMC Infect Dis. 2013;13:78.